Compare and contrast type 1 and type 2 diabetes and summarize the recommended nutrition therapy for each.
What will be an ideal response?
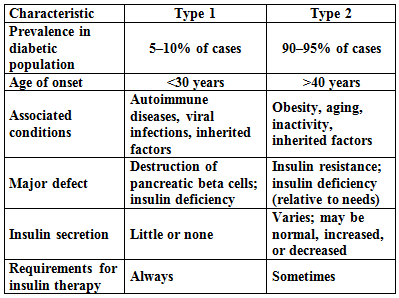
In type 1 diabetes, the less common type (about 5 to 10 percent of all diagnosed cases), the pancreas loses its ability to synthesize the hormone insulin. Type 1 diabetes is an autoimmune disorder. In most cases, the individual inherits a defect in which immune cells mistakenly attack and destroy the insulin-producing beta cells of the pancreas. The rate of beta cell destruction in type 1 diabetes varies. In some people, mainly infants and children, destruction is rapid; in others (mainly adults), it is slow. Type 1 diabetes commonly occurs in childhood and adolescence, but it can occur at any age, even late in life.
Type 2 diabetes is the most prevalent form of diabetes, accounting for 90 to 95 percent of cases. The primary defect in type 2 diabetes is insulin resistance, a reduced sensitivity to insulin. Consequently, muscle and adipose cells cannot remove glucose from the blood, and blood glucose remains elevated. To compensate, the pancreas secretes larger amounts of insulin, and plasma insulin concentrations can rise to abnormally high levels. Over time, the pancreas becomes less able to compensate for the cells’ reduced sensitivity to insulin, and the hyperglycemia worsens. The high demand for insulin can eventually exhaust the beta cells of the pancreas and lead to impaired insulin secretion and reduced plasma insulin concentrations. Type 2 diabetes is therefore associated both with insulin resistance and with relative insulin deficiency; that is, the amount of insulin is insufficient to compensate for its diminished action in cells.
This table summarizes the differences and similarities between type 1 and type 2 diabetes.
Nutrition therapy for type 1 diabetes focuses on maintaining optimal nutrition status, controlling blood glucose, achieving a desirable blood lipid profile, controlling blood pressure, and preventing and treating the complications of diabetes. In addition to meeting basic nutrient requirements, the diet must provide a fairly consistent carbohydrate intake from day to day and at each meal and snack to help minimize fluctuations in blood glucose. Further alterations in diet may be necessary for a person with chronic complications such as cardiovascular or kidney disease.
In overweight people with type 2 diabetes, even moderate weight loss (5 to 10 percent of body weight) can help improve insulin resistance, blood lipids, and blood pressure. Together with diet, a regular routine of moderate physical activity not only supports weight loss, but also improves blood glucose control, blood lipid profiles, and blood pressure.
You might also like to view...
What specific signs and symptoms noted with Mrs. Washington's exam and history are consistent with her diagnosis? Which symptoms place Mrs. Washington at nutritional risk? Explain your rationale
What will be an ideal response?
Explain how hepcidin controls the level of plasma iron.
What will be an ideal response?
Which of the following techniques for measuring body composition makes use of small exposures to radiation??
A) ?MRI B) ?DEXA C) ?TOBEC D) ?BIA
The only cells which do not contain mitochondria are the red blood cells, which produce energy ________ in the cytoplasm
A) aerobically B) anaerobically C) rarely D) often